5 ways to improve patient care delivery and increase value-based pay contracts for private-duty nursing & pediatrics
Everyone with medically complex needs or chronic conditions deserves high-quality, patient-centric care that is comfortable and outcomes-focused.
82% of patients also say that quality customer service is the most critical factor to satisfaction with the care they receive. Patients and their families seek care workers and nurses who understand their needs and can communicate effectively.
Patient satisfaction with the care they receive is the main focus of value-based care. However, only about 35% of organizations currently have value-based pay (VBP) contracts with Medicaid funders in the United States.
VPB contracts are beneficial for patients and providers alike. However, securing these contracts can be challenging for organizations lacking the necessary data, technology, and strategies.
In our recent webinar, Harvey Mathews, co-founder and COO of First Day Homecare, and Kayla Raimondo, Market Leader for Skilled Nursing at AlayaCare, discussed strategies for improving patient outcomes in private-duty nursing and pediatric home-based care. They highlighted key practices, market insight, and trends that organizations can consider to enhance care delivery and obtain more VBP contracts.
5 strategies for improving patient outcomes and boosting VBP contracts

1. Understand Electronic Visit Verification (EVV) and compliance for your organization
Electronic Visit Verification (EVV) is a system that requires visits for Medicaid-funded personal care, home health, and private-duty nursing services to go through a state aggregation system. It is primarily used as a pre-or post-payment validation system. Care providers are required to capture and share using an EVV-compliant system or to send to the corresponding EVV state aggregator. This allows claims to be matched with the actual care provided in the home.
EVV is vital for value-based care because it ensures that high-quality care services are delivered at the right time, to the right person, and by the right provider. It ensures that services are rendered as planned and allows for real-time tracking of care delivery. It confirms that contracted services are provided and contribute to patient electronic health record data. This integration ensures that all care activities are documented, promoting a holistic view of the patient’s health status and care interventions [ref].
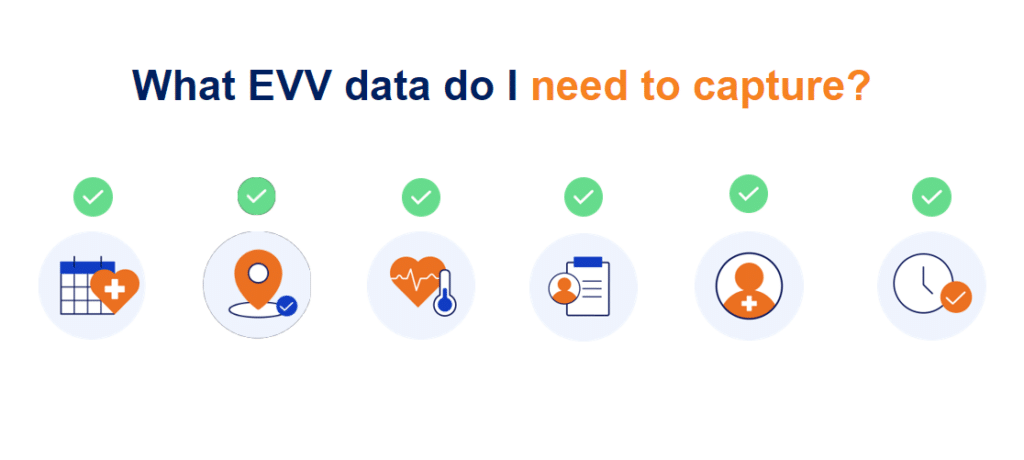
Want to know how EVV impacts your organization? Watch the webinar at 10:29 as Kaila explains the steps to determine whether EVV impacts your organization, what EVV data to capture, and any other important considerations.
2. Determine the right tech to support the mandates and changes
The key considerations you should remember when determining if you have the right technology depend on whether your state follows an Open or Closed EVV model.
In an open EVV model, states allow providers to use their existing EVV system or choose one that best meets their individual needs. This means you should assess whether your current software solution effectively tracks and captures the data needed for EVV billing, including the six EVV data points Kaila mentioned in the webinar. [click to watch]
Additionally, when evaluating technology solutions, consider if your software provider allows you to track EVV data directly in their platform, how easy it is to train your staff on staying compliant, and what guardrails the platform has in place to ensure data accuracy when your frontline staff delivers care.
While most states follow an open EVV model, states that follow a closed EVV model will contract out a single EVV vendor, mandating all providers to use that system for capturing EVV.
Here’s an example from First Day Homecare on how they found the right technology for their EVV needs:
Before implementing AlayaCare, First Day Homecare manually verified every visit, consuming extensive staff time each morning for compliance and accuracy, including coordinating with nurses to confirm exact times. About nine months ago, they switched to AlayaCare’s visit verification system, allowing them to set custom rules to identify issues like late arrivals, early departures, or overtime by nurses.
This change has improved their morning verification success rate to 80%, significantly reducing the need for manual checks from 100% to just 20% of visits. Most issues now flagged are minor and often pre-communicated by nurses, such as working an extra hour. This shift to AlayaCare has dramatically decreased the manual effort required for visit verification. First Day Homecare expects further reductions in manual reviews as they refine the process.
Adopting AlayaCare has notably decreased the time and effort dedicated to visit verification.
3. Optimize coordination and care continuity
Optimizing coordination works hand in hand with enhancing the patient experience. Using technology to streamline coordination and care continuity ensures that nurses understand their daily schedules and where they will be at any given time while optimizing routes to reduce mileage and travel time on those patient services. Additionally, the right technology can ensure that you can maintain care continuity with the patients you serve, which is critical to ensuring a better patient experience.
For example, AlayaCare’s Visit Optimizer tool matches nurses with patient visits based on skillsets, proximity, and other criteria to ensure a balanced workload, minimize travel time and costs, and maximize direct patient care.
Documentation efficiency is also vital to optimizing coordination and maintaining care continuity. Nurses should have access to everything they need to know about a patient and their care plan before their visit. Effectively balancing clinical documentation and the patient experience patient interaction is key to better care delivery in the home.
“Improved care worker experience will also, by proxy, improve your client experience. If nurses are excited to come to work, to care for their patients, and feel their technology enables them to do so, less time will be spent documenting in the home, and more time will be spent providing care to those respective patients.”
— Kayla Raimondo, Market Leader for Skilled Nursing at AlayaCare.
4. Utilize communication and patient engagement tools
“Patients want to be supported and feel as though they have the level of comfort that, let’s say, a private nursing home would provide with that twenty-four-hour care but in the comfort of the places they call home.”
— Kayla Raimondo, Market Leader for Skilled Nursing at AlayaCare.
Communication and patient engagement tools can provide patients and nurses with real-time visibility. If an adverse event occurs, you can intervene immediately, reducing the risk of hospitalization.
A patient and family portal is an example of a communication and patient engagement tool that can make care plans and necessary information, such as all information from past visits, documents, and other essential details, easily accessible for patients and their families. It empowers patients and their families to stay active in their care plans and can be used as a secure way to contact and provide feedback to providers quickly.
“Our nurses and the families love having access to all that data. They find it extremely helpful, enabling them to contact us quickly. We appreciate [our patients] candid feedback.”
— Harvey Mathews, co-founder and COO of First Day Homecare.
The key to better client experience? Improving communication between home-based care providers and clients

5. Utilize technology for outcomes and data reporting
Leveraging technology can help organizations gather the data required for those value-based contracts while improving the patient experience. It ensures that you analyze those clinical trends, measure outcomes, and ensure patients have the highest level of care possible with the services you provide. For example, AlayaCare’s custom forms tool allows providers to gather data they need to eventually report on essential clinical information and track progress toward care plan goals.
“It is enabling you to create and then slice and dice the data as you see fit with all of the data points, even the custom ones,”
— Kayla Raimondo, Market Leader for Skilled Nursing at AlayaCare.
4 data reports to drive better client experience and satisfaction

AlayaCare is an end-to-end private-duty nursing platform that creates an integrated care network between back-office staff, field nurses, and patients and their families. To discover how AlayaCare can improve care delivery and patient outcomes for pediatrics, tune into our latest webinar below!
First Day Homecare is a leader in professional in-home care for children and adults throughout Michigan and beyond. They have been a trusted partner for years, utilizing the AlayaCare platform to provide private-duty nursing services across pediatric, geriatric, and chronic care patient populations.
Learn how AlayaCare supports First Day Homecare to deliver top-tier private-duty nursing and pediatric services.
The post 5 ways to improve patient care delivery and increase value-based pay contracts for private-duty nursing & pediatrics appeared first on AlayaCare.